Chapter 4: Treating obstructive sleep apnea (OSA) with CPAP and dental appliances.
Treating obstructive sleep apnea (OSA)
OSA is the most common type of sleep apnea, and it is no laughing matter.
Or rather, it is a “no-breathing matter” since that’s what apnea means.
Have you just been diagnosed with OSA and you want to understand what therapies are available?
Or maybe you only want to learn about this common disease’s therapeutic strategies and which ones are more effective?
Whatever your motivation for being with us today, I assure you that you have come to the right place.
With over 10,000 words and 49 sections, this article will cover every single lifestyle treatment that currently exists.
This includes also dental appliances and continuous positive airway pressure.
If you want to learn about surgical treatments instead, check Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.
If you are an OSA patient or some people dear to you suffer from this disease, you will be relieved to know that several strategies exist that can treat OSA.
So, without further ado, let’s dive into the article.
How do you treat obstructive sleep apnea (OSA)?
Quick: are medicines the most frequently used treatment of OSA?
…. Yes?
Nope, they are only rarely used.
Sleep apnea is typically treated with:
- lifestyle changes such as losing weight, quitting smoking, …. These may be effective in mild forms of sleep apnea;
- mouthpieces such dental appliances, which may relieve mild sleep apnea;
- breathing devices, such as continuous positive airway pressure, which are more suited for moderate or severe sleep apnea;
- surgery that is used for moderate or severe sleep apnea.
What are the objectives of treating sleeping apnea?
If you thought that the treatment’s purpose is to make breathing more comfortable, then you guessed right.
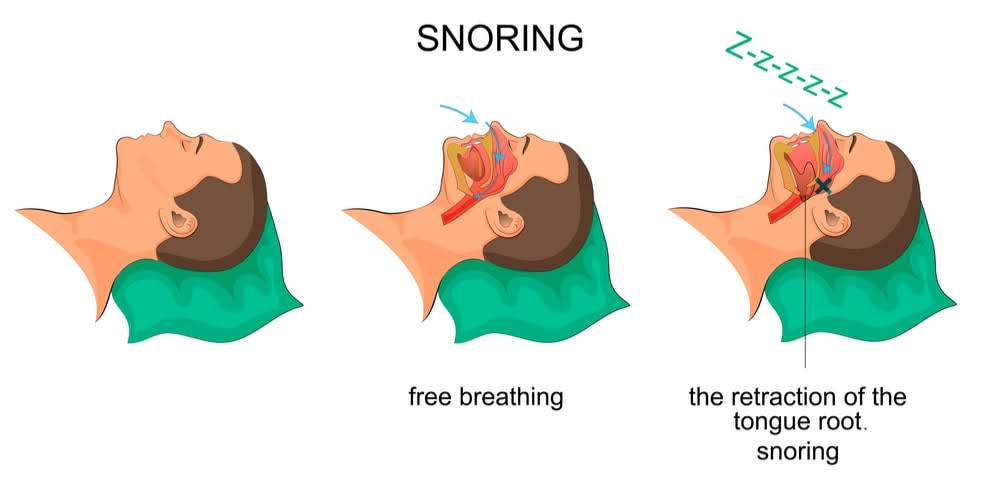
Indeed, the objectives of treating sleep apnea are always the same: hold open or increase the size of the upper airways’ opening during sleep.
The goals are two-fold:
- improve the quality of your sleep, eliminating apneas and hypopneas and thus increasing blood oxygen levels;
- reduce symptoms like snoring, sleepiness, enhancing the quality of life.
Treatments may also improve other medical issues associated with sleep apnea such as:
- High blood pressure,
- stroke,
- heart disease,
- and diabetes.
and they can also reduce the risks of suffering from these diseases.
Let’s now look at what you can do.
What lifestyle changes can you implement to treat mild sleep apnea?
If you suffer from mild forms of sleep apnea, then it may be possible to treat it merely with some lifestyle changes:

- If you are obese or overweight, your risks of suffering from sleep apnea increase. Even a mere 10% weight loss can be beneficial and relieve your symptoms Experts believe that excess body weight may contribute significantly to sleep apnea.
Losing weight is not easy! Studies have shown that if you are obese or overweight, going on a diet (and losing weight) will be beneficial since:- your apnea frequencies will decrease;
- your Apnoea–Hypopnoea Index (AHI) will improve compared to controls.
- If you are a smoker, you also need to quit tobacco consumption. Smoking irritates your throat and makes you cough at night.
- Avoid alcohol, sleeping pills or painkiller drugs. They make it harder for your throat to stay open while you sleep since they relax throat muscles.
- Sleep on your side instead of your back. This may reduce sleep apnea symptoms. Sleeping on your back in fact stretches your throat and neck’s tissues, thus narrowing or blocking your upper airways. You can learn to sleep on the side by placing a pillow so that it may support you (on the side). You could also use the ‘tennis ball trick’: sew a pocket onto the back of your pajama top and put a tennis ball in it. The pressure from the ball will make you roll back to your side.
- Practice sports regularly. Also, try to have regular sleep patterns by going to bed and waking up more or less at the same time. This will improve the quality of your sleep.
- Do you have a runny or stuffed-up nose, because of an allergy or a cold? If so, then consider using some nasal sprays or allergy medicine. Check with your treating physician what is the best treatment for you
We will now look at the use of medical devices that can help your OSA.
Dental appliances
Are dental appliances behavioral treatments
You can consider mouthpieces, also called dental appliances, as behavioral treatments.
Why?
Because they have to be worn regularly to re-align the oral cavity. Hence, they lead to a change in your behavior.
The American Academy of Sleep Medicine (AASM) recommends them as:
- A first choice therapy in mild or moderate forms of sleep apnea.
- Severe forms when CPAP has failed or where patients prefer alternative therapies. But they are not the first choice for severe forms because they may not be enough for a challenging airway
They are also used:
- Concomitantly with CPAP to lower the air pressure levels, if you do not tolerate higher pressures.So there is hope if you struggle with CPAP!With the help of a dental appliance, your airway will present less resistance. Your CPAP machine will, therefore, blow air with lower pressure and more timely;
- if you have refused or failed surgery (such as tonsillectomy, adenoidectomy, …).
Your doctor may recommend them if you snore loudly, even if you do not have sleep apnea.
Let’s now look at how dental appliances can treat your sleep apnea.
How do mouthpieces treat sleep apnea?

To understand how they work, let’s see how you wear them.
Can you picture an orthodontic retainer or a sports mouthguard?
Dental appliances to treat sleep apnea look similar.
Most of them rely on the principle of mandibular advancement.
OTC dental appliances are made out of two parts:
- one latches onto your upper teeth,
- the other, onto your lower teeth.
The bottom part maintains your lower jaw in an advanced position making your breathing more comfortable.
Your tongue is also adjusted to keep your upper respiratory airways, in the back of your throat, open.
This facilitates airflow and reduces snoring and OSA.

Dental devices made ad-hoc by your dentist, to treat OSA, differ somewhat from their OTC counterparts since:
- the part fitting over the upper teeth and over the lower teeth connect via metal hinges, with a piston and tube;
- they are usually adjustable so that your dentist can gradually change your advancement to get the best results;
- when your muscles relax, the piston and tube limit the tendency of the jaw to move backward;
- When you fall asleep, and your muscles relax, your chin is kept forward, and your airways stay open.
Another type of dental appliance is also used where your tongue protrudes instead of your lower jaw.
It will maintain your tongue forward by suction, preventing it from occluding your upper airways.
But, since they are not well tolerated, they are not part of the current recommendations for oral appliance treatment.
Let’s now learn about the different types of dental appliances available in the market.
… jump on to the section to find out!
Different types of dental appliances
Quick, how many different types of dental appliances are there in the market?
….. hundreds of over-the-counter models are available.
To that, you need to add the custom fitted devices.
Who can make ad-hoc dental appliances?
A dentist or an orthodontist who is a doctor specialized in improving your bite by correcting teeth or jaw problems.
And they can make appliances for all types of patients, for all sorts of oral anatomies including patients without teeth.
Even though many models are available, their underlying principle is the same:
- they exert traction on soft tissues,
- to free the upper airways,
- and ease airflow.
Move on to the next sections, if you wish to learn more about the pros and cons of the different dental appliances used to treat OSA.
Over-the-counter (OTC) dental appliances
Price!
Yes, that is the only main advantage of over-the-counter dental appliances.

But that comes with other types of costs because prefabricated oral appliances:
- May fall out at night and your snoring will continue.
- Have to fit different anatomies and tend to be bulky. To understand how they work, let’s see how you wear them.What a paradox! A bulky dental appliance in a small airway!Indeed, it will be challenging to improve your snoring and sleep apnea.
- May mislead you, or rather, their results may mislead you.If you are successful at eliminating snoring symptoms and think that your sleep apnea has been cured….you may suffer from the complications of an untreated sleep apnea later on. And OSA is no laughing matter since it is a life-threatening disease. Also, your jaw position may actually be worse and increase occlusion of the airway without you realizing it.
- may force you to clench to keep the dental device in place.
But a sleep medicine trained dentist will immediately identify these issues, and help you avoid them.
The ease with which you can buy OTC appliances may fool you into thinking that:
- you can diagnose your sleep apnea,
- and manage its side effects on your own.
Fortunately, some of the above issues, namely lack of comfort (and even pain), limit their use somewhat.
And this despite that they have been around for approximately 20 years.
One of the paradoxes of their lack of effectiveness and discomfort is that …..
………they discourage patients who would otherwise be excellent candidates for custom-fitted appliances.
Let’s see how you can use them, to better understand some of the issues.
OTC dental appliances: less than optimal fit
Many of these OTC appliances are crudely made with thermoplastic polymer materials.
When you buy them, you often need to boil them.
No! No sauce needed ? (we are easily amused with simple jokes here at SPDA).
They are softened by boiling so that they mold and adapt to your oral anatomy when you bite the softened material.
You will do this with a somewhat advanced jaw position.
No wonder these appliances are also called “boil and bite.”
The appliance is then placed in a bowl of cold water to “set up.”
The end result is a device that may somehow fit, but it is not always a very good fit.
Now let’s analyze how an optimal fit is ensured when a qualified dentist gets involved:
- he will take an impression and send it to a lab;
- once the oral appliance is received, your dentist will make the necessary, delicate adjustments to achieve an optimal fit;
- these adjustments will depend on your OSA symptoms and oral condition.
These are all chair-side steps which need time and engender costs.
It is important to note that, in New York, a dentist has to:
- attend courses
- and receive training
to make custom appliances for sleep apnea and snoring.
Doctors have to follow with rigorous standards ensuring good success rates.
It is thus preferable to contact your dentist to have a dental appliance really adapted to your anatomy (teeth and gums).
Let’s now study what happens as you get older.
Poor to no adjustability of OTC dental appliances
How will your sleep apnea evolve as you age?
It is likely not be shocking if I tell your that your sleep apnea will get worse.
That happens because muscles lose their tone, and tend to occlude your airways.
Though it is true that you may compensate for this process by losing weight, for instance.
This may improve your OSA.
But, the prevalent trend shows an increase in the severity of sleep apnea as you get more mature, so to speak.
Now, one of the significant benefits of your custom-made device is that it can be adapted.
You will thus be able to incrementally advance your jaw over the years as the aging process takes its toll.
This also comes in handy when you are just beginning to use the device.
The first few weeks your dentist will gradually move your jaw forward. This will help to avoid pain from a sudden and abrupt advancement.
But OTC models do not offer this benefit.
Longevity of OTC dental appliances.
Is there a difference in durability of a prefabricated dental appliance versus a custom made one?
The answer is a definite yes, and the difference is significant:
- The former lasts only a year approximately,
- the latter has a lifespan of 2-5 years. The time depends on whether you clench and grind your teeth during your sleep.
Finally, the AASM and the AADSM guidelines also advise that:
…… “a qualified dentist uses a custom, titratable appliance over non-custom oral devices.”
This means that an adjustable (titratable) oral device should be used.
Can I use Medicare approved OTC dental appliances?
Yes!
Do you definitely want to try an OTC dental appliance instead of one made ad-hoc for you? If so, then go for a Medicare-approved one.
They have been tested clinically and also stand the test of time.
It will be a safe choice that may protect you from some of the issues explained above.
What are the advantages of dental appliances versus CPAP masks?
Amongst the pros …..

- Dental appliances can significantly reduce sleep apnea, if used over an extended period. And, you will show better adherence to treatment because mouthpieces are more comfortable to use than CPAP masks. Unlike CPAP masks, they:
- are portable hence you can travel with them;
- allow you to talk and drink water.
- You will not have any dry, itchy nose issues due to air pressure from a CPAP mask.
- Itchy Nose Oral appliances are less cumbersome to use than CPAP equipment
- If you move a lot in your sleep, there no risk of getting entangled with the tubing because there is none;
- a dental appliance will stay in place until the end of your sleep. That is unlike CPAP masks which you may unintentionally remove;
- finally, a dental appliance does not need a machine.
Let’s now take a look at the cons of oral devices.
What are the disadvantages of dental appliances used to treat OSA?
To begin with … These can be permanent or transient.
I know what you are thinking!
You would prefer the side effects of oral appliance therapy to be transient only and not permanent.
But do not worry.
The benefits of oral appliance therapy outweigh the adverse effects.
This is what the majority of patients have said.
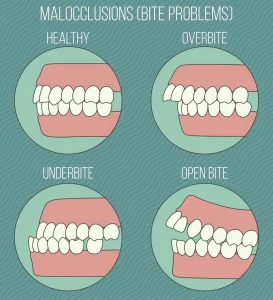
Permanent effects include dental changes that occur over the long term due to the pressure exerted by your dental appliance.
They won’t have a significant impact on your chewing, and you will not even be aware of differences to your bite.
Though, tooth movement is observed in 85,7% of patients according to a 5 years analysis
The types of tooth movement that you may experience include, for instance, a decrease of the overlap of your lower teeth by your upper teeth (aka overbite).
And this may not always be a bad thing ? !
Other observed changes include:
- A decrease in the number of contacts between teeth’s surfaces (occlusal contacts);
- forward inclination of the lower incisors and backward inclination of the upper incisors;
- Etc.9
Exercise caution though, if you have been recently treated by an orthodontist these changes may be more noticeable.
While the above is true, you can prevent these issues with proper preventive jaw exercises.
You should do them in the morning.
They will decrease the risk of teeth displacement.
Also, worthy of notice is that CPAP masks as well, may displace teeth via the pressure exerted on the upper teeth (see What are the effects of CPAP therapy on your jaws and teeth?)
Let’s now look at transient side effects.
Their frequency varies significantly amongst patients.
They occur during the first two months of the therapy and include:
- Headaches
- A toothache
- Gum inflammation
- The pain of the muscles that move the jaw (temporomandibular joint discomfort)
- Dry mouth
- Excessive salivation
Your situation may worsen if:
- you already suffer from jaw pain,
- or from pain in the temporomandibular joint (TMJ)
before starting the treatment.
Though, do you want to know the best part?
Interestingly, you will discover that, against expectations, improvements are sometimes observed from the start.
How is that possible?
… jump to the next section to find out.
Of sleep apnea, teeth grinding and oral appliances
So, why may jaw pain or pain in the temporomandibular joint (TMJ) improve when using a dental appliance to treat sleep apnea?
This has a simple explanation!
If you observe relief of pain after using the appliance, then it came from your teeth’s grinding. This is also called bruxism and occurs during your sleep.
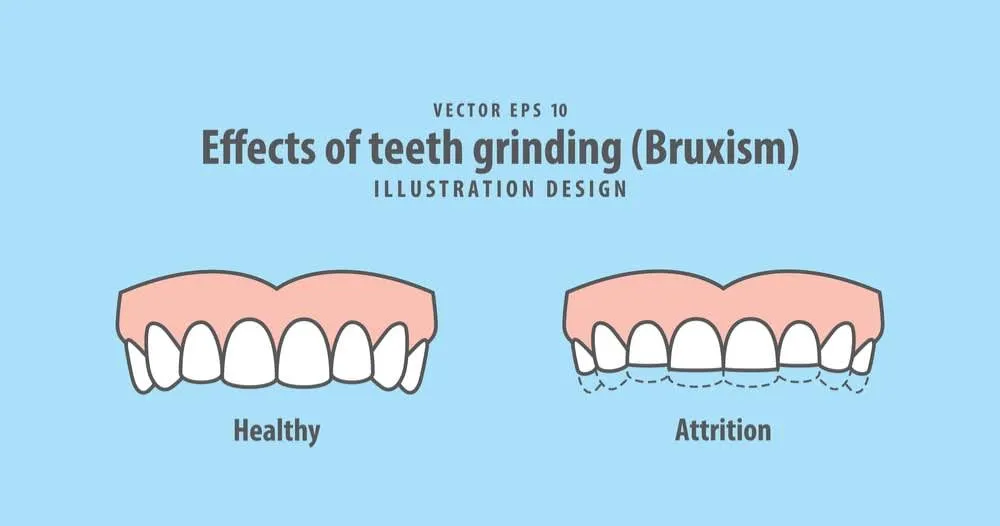
And it does not come by chance.
It is related to your sleep apnea.
Let me explain that.
It is your body’s instinct to trigger a back and forth motion (associated with teeth grinding) to keep the airways open when your muscles relax during sleep.
Hence the cause of your grinding and excessive use of the jaw muscles is sleep apnea.
Treating sleep apnea with a dental appliance may solve all these issues.
Now, teeth grinding and clenching comes at a cost:
- poor quality sleep,
- jaw popping,
- headaches,
- gradual teeth erosion and destruction,
- jaw pain,
- neck aches.
So I am sure you agree, treating it will be quite a relief.
As a side note, be wary of nightguards!
Does that surprise you?
It should not!
These are prescribed to protect your teeth from erosion during grinding and clenching (bruxism).
But what if your bruxism is not due to stress but rather to a small airway passage?
Then the following will probably happen:
- your small airway will become even smaller,
- its blockage will increase,
- so will your teeth grinding,
- and your sleep quality will further deteriorate.
So, make sure your dentist rules out sleep apnea before prescribing a nightguard.
If you suffer from sleep apnea then you doctor should focus on its treatment first.
One last word of caution.
While the above holds true, the relationship between OSA and sleep bruxism is not always clear.
Sometimes, patients successfully treated for sleep apnea with a dental appliance may continue teeth clenching and grinding.
In these cases, your dentist should consider a reinforced adjustable mandibular device. It will avoid breakage of your oral appliance.
Some patients have been reported to break their oral device during sleep bruxism
Okay, it is now time to talk about the clinical results of oral appliances therapy.
How effective is a dental appliance to treat sleep apnea and snoring?
If you snore, you will be happy to know that response rates are high, almost 95%!
And that is really good news!
Because snoring either disappears entirely or it decreases to acceptable levels.
And if you suffer from sleep apnea, you have approximately a 67% chance of seeing a significant improvement of your sleep apnea.
There is substantial evidence that the majority of patients benefit from dental appliances. This also includes some with more severe disease.
But it is not possible to predict in advance whether treatment will be successful.
Studies show a range of positive responses between 50-80%.
Why this difference?
It really depends on:
- the study,
- the criteria used to assess responses,
- patients’ selection criteria.
For instance, if you are a patient who can breathe well through the nose, then you will be able to use your dental appliance more efficiently, and the results will improve.
The results obtained with a dental mouthpiece also improve if you are a woman because women respond better.
European studies tend to include thinner patients than USA ones. And it is well known that your weight directly influences response to a dental appliance.
Also, if you are thin, you will respond better to dental appliances.
Why do you think?
Well, because your neck’s size is smaller and your lower jaw bones don’t sit too far back.
Let’s now take a peek at how treating sleep apnea and snoring differ.
Dental appliances: how does treating snoring differ from sleep apnea?
Freeing your airways by moving your jaw forward …
… That is the purpose of dental appliances whether you snore or you also suffer from sleep apnea.
At the start, treatments are similar, and your dentist may even use the same appliance.
But that’s where the similarity ends.
Treating snoring is shorter and less complex than treating sleep apnea.
Often, if you are a sleep apnea patient, you may be relieved from snoring symptoms while still suffering from sleep apnea.
If you suffer from sleep apnea, your dentist will continue to use the dental appliance to re-align your oral cavity until:
- You feel better, are less tired, etc..
- or until you reach the maximum advancement you can tolerate.
How can I know if using an oral appliance will decrease my sleep apnea?
Knowing if you are likely to respond would be a considerable time and cost saver … I am sure you would agree.
And surely it would be a highly desirable outcome because:
- The success of treatment with dental appliances is lower than that of CPAP;
- the process is also more time consuming and costly than CPAP.
But life is not always easy!
Despite many studies, no standardized parameters or procedures exist to gauge response before manufacturing a dental appliance.
While the above remains true, some factors are associated with treatment success, these include:
- OSA observed during supine sleep,
- low apnea-hypopnea index,
- young age,
- female patients’ compliance,
- obstruction area mainly involving the oropharyngeal region,
- small neck circumference,
- low body mass index.
Though, beware! … none of these factors, either singly or in combination, can predict a positive outcome when treated with a dental appliance.
So, oral appliances are not the be and end all of OSA treatments.
Now, let’s investigate when you can, or cannot, use them.
Can you always use an oral appliance if you suffer from sleep apnea?
Unfortunately not!
Although this may seem surprising, the reason is simple: you require a healthy dentition for dental appliances therapy.
Your oral health may thus be a barrier to the use of such devices.
So, what is the solution?
Well, there are three possibilities:
- You may have to delay the use of an appliance. You should do that until you have received appropriate dental treatment and your oral health has improved.
- Or you may start oral appliance therapy while requiring close supervision and follow-up. This will avoid worsening of previous dental or temporomandibular joint issues.
- You may also not be a good candidate for it.
This is especially true for older patients.
Let’s look at some examples of oral health issues.
Dental health problems to consider before using a dental appliance for OSA.
Just like taxation is a certainty in life, some dental health issues will invariably affect your use of dental appliances.
Let’s look at these dental health concerns.
Tooth loss
It is associated with sleep apnea.
If you are an edentulous patient, you will be more likely to suffer from sleep apnea. A study found that if you were a patient aged 25-65, your risk of developing OSA would increase by 2% for each additionally lost tooth.
So, your dentist will have to carefully consider restoring your missing teeth, before an appliance is made.
This will create a more balanced occlusion.
Likewise, use of dentures is associated with a higher apnea-hypopnea index (AHI>15).
Chronic what…
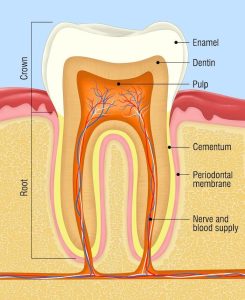
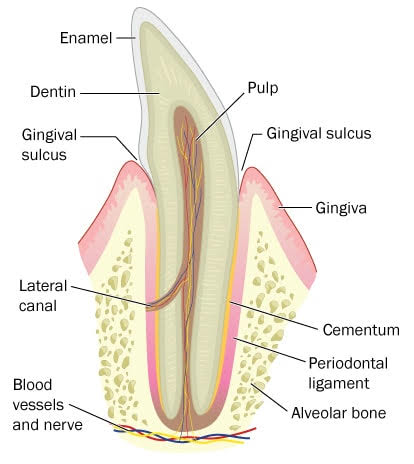
Here below is a brief explanation and some useful images.
It is the inflammation of your periodontal tissues. They include:
- the gum tissues covering your alveolar bone;
- the alveolar bone which supports your teeth. If it is unhealthy, then it will no longer support them, and you will suffer from tooth loss;
- your periodontal membrane which can be found between your teeth and your alveolar bone.
This disease is a significant issue among patients undergoing oral appliances therapy. This is because teeth may be pulled out as your appliance protrudes your lower jaw forward.
A study found that you are more likely to suffer from periodontitis if you also have OSA.
Dry mouth
As you may have already guessed, it results from an insufficient salivary function.
It is a frequent symptom among sleep apnea patients.
It is also a sign of poor oral health.
How do we know that?
Because these same patients also have:
- more pain associated with dentures,
- fewer teeth,
- more caries,
than the normal population
Indeed, saliva is not just your precious ally if you play the chatterbox, for it regulates pH in the oral cavity. Acidic compounds are thus less likely to damage your teeth.
Also, you may not know that …
…. saliva production is lowest during sleep and it will be worse if you are an OSA patient.
Why?
Because OSA patients tend to breathe through their mouth.
Teeth grinding and clenching
Last but not least comes bruxism.
Can you guess when and why your dentist will be very concerned?
When you have dental prosthesis – that answers the first question.
And for the second question, the reason should be obvious after reading the first answer….. bruxism damages prosthesis.
That is why he will prescribe a bite guard covering your superior dental arch.
Unfortunately, this is mostly done without a sleep study despite the frequent concomitance of sleep apnea and bruxism
A study analyzed the impact of such guards on patients with sleep apnea and the results found were worrying:
- the apnea-hypopnea index increased by >50% in 5 of 10 patients
- the sleeping time with snoring increased by 40%.
So, the risk of aggravation of your sleep apnea is a reality when you wear a dental guard (see also Of sleep apnea, teeth grinding and oral appliances).
Which dental devices for OSA patients with insufficient dentition?
If you have been an avid reader of the previous sections, then you will probably conclude that:
then surgery is the only treatment left?
Not so fast! You can use a different approach that does not need teeth for retention: a tongue retaining device.
This comes in handy if:
- you are receiving dental treatment,
- and if you do not have enough dentition to use a mandibular advancement device.

So, what does it do and how does it work?
- It manages to maintain your tongue in a forward position by suction.
- It looks a bit like a pacifier with a flexible bulb positioned in front of your mouth.
- First, you need to protrude your tongue so that it goes into the anterior bulb.
- Next, you have to give the bulb a little squeeze.
- This results in a suction that holds the tongue in a forward position.
Some of these appliances are prefabricated, like the tongue-stabilizing device (TSD). Others are custom made instead.
But what about if your tongue does not extend beyond the lips?
Good call!
Then, unfortunately, this solution will not be suitable.
Let’s now take a look at how technology is being used to innovate.
Oral devices to treat sleep apnea: technological advances
Indeed, technology is here to surprise you!
During the last few years, remotely controlled mandibular positioners have been introduced.
They can:
- identify whether you are a responder
- assess the degree of mandibular advancement necessary for you. This requires a polysomnography test during one night.
Also, some new generation dental appliances feature some small temperature sensors. They assess your adherence to treatment.
Let’s now delve into the most frequently used treatment of sleep apnea.
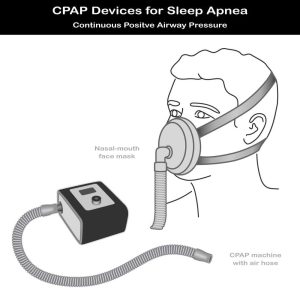
Continuous positive airway pressure (CPAP)
What is continuous positive airway pressure (CPAP)?
Before oral appliances came into use, CPAP was the only medical device available.
And it is still the most popular and also the primary treatment of sleep apnea.
It prevents your upper airways collapse during your sleep.
But how does it work?
By providing a constant flow of pressurized air that is gently blown into your respiratory airways. This serves to keep them open while you sleep at night.
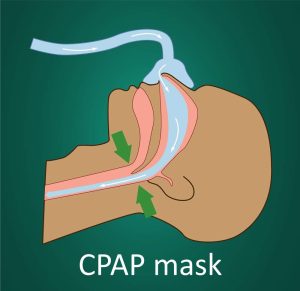
The mask must ensure a good seal.
If this is not the case, air leaks may lead to insufficient air pressure with suboptimal results. Your airways may not open because of insufficient air pressure.
You can use both a mask, fitting over your nose and mouth, or a nosepiece (only) fitting over your nose.
Flexible tubing is connected to the mask and to a machine. This tubing is long enough to ensure you are comfortable (you can turn or move easily).
When you use a CPAP machine, you will see that these devices:
- are portable hence quite small (the size of a tissue box)
- can be easily placed next to your bed, for instance on your nightstand
- blow ambient air into your trachea
- are equipped with a humidifier to moderate air
- are also equipped with a chip card. This serves to record events occurring during your sleep (micro-awakenings etc..).
CPAP types of equipment have improved and continue to improve.
They are becoming more and more user-friendly, less cumbersome, quieter and less intrusive.
Though, being hooked up to a machine… well, it is not very attractive, is it?
That leads on nicely to the next question.
How long should I use CPAP for?
Let’s address the elephant in the room.
You are wondering, and that is only human, whether you will have to use it forever.
Indeed, the thought of having to use CPAP for the rest of your life is not very reassuring. It is not the most appealing treatment for sure!
But you may not have to.
It really depends on the cause of your sleep apnea, and that is person dependent.
Factors that lead to sleep apnea include:
- loss of muscle tone due to aging, for instance, menopause.
- As you get older, teeth position may also change. These may affect the airway and how well you can breathe during sleep.
- Reversible factors where you will experience sleep apnea in specific contexts or where it is aggravated by others:
- Sleeping on your back,
- REM sleep,
- after alcohol consumption,
- becoming overweight since the accumulation of fat at the base of the tongue narrows your airway,
- nasal congestion due to a cold or allergies,
- pregnancy especially for women who are overweight or obese, or who gain excessive weight during pregnancy.
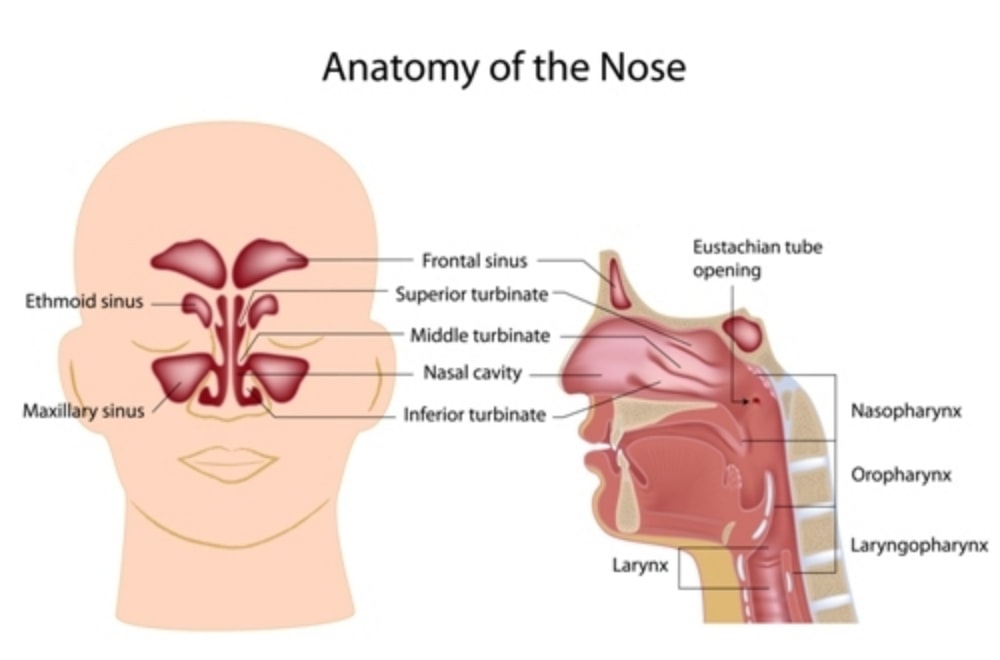
- Anatomy of the structures within your throat, nose, position of your tongue and jaw:
- Inflammation of your turbinates (tissues within your nose) due to infections, allergies, weather, and temperature changes …
- A broken nose can lead to a deviated septum and increase the chances of suffering from sleep apnea.
As you can see, some of these causes can be corrected.
For example, if you lose weight, your sleep apnea may likely improve.
The same is true if you undergo surgery to correct a deviated septum or get treatment for your allergies.
Hence doing CPAP is not like serving a life sentence.
How about the frequency of use?
Should you use it every time you doze off?
Move on to the section to find out.
How often should I use CPAP?
Unfortunately, the answer is short and clear: you should use it every time you sleep.
It is a lifestyle change.
Why such frequent use?
Because the more you use it, the better you will feel and you will decide it is worth putting up with the inconvenience.
One night without CPAP can:
- Negatively influence your quality sleep
- increase your blood pressure
- decrease your daytime alertness and function
- etc.
But how effective is CPAP at treating sleep apnea?
Let’s see…
How good are results obtained with CPAP?
CPAP does work!
It will reduce or eliminate:
- Sleep apneas or hypopneas, so that you will no longer snore or make choking sounds when you sleep.
- Fragmented sleep due to micro-awakenings because of lack of oxygen.
But that is not all!
By eliminating sleep apnea, you will also have many other health benefits:
- less sleepiness hence better daytime alertness,
- better memory and thinking skills, better concentration throughout the day,
- lower risks of motor vehicle accidents (see also Does OSA increase the chance of a motor vehicle accident?),
- lower risk for diabetes (see also How are OSA, diabetes Type 2 and cardiovascular diseases related),
- you will feel emotionally more stable, and your risk of depression will be lower.
And, using CPAP therapy over an extended period can protect you from cardiovascular problems. Hence, your risk of dying from:
- Stroke,
- congestive heart failure,
- coronary artery disease,
- irregular heartbeat,
will decrease (see also Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects).
Now gentle reader, maybe that after reading this you are leery that there is a price to pay for these positive effects.
And you are right because CPAP has some adverse effects.
But before we look at its side effects, let’s learn about the results obtained with some of OSA’s associated diseases.
Does treatment with CPAP influence hypertension in OSA patients?
Several studies have been done to answer this question.
Now, despite variations of CPAP’s effects, results seem significant. A decrease in arterial pressure will be more important if you:
- have a severe OSA,
- are obese,
- are treatment compliant, in other words, if you stick to treatment.
Let’s now talk about how CPAP’s treatment of OSA affects associated coronary heart disease.
Is it beneficial to treat OSA with surgery or CPAP if you suffer from coronary heart disease (CAD)?
This time, a study on 54 CAD patients provides some interesting answers.
Are you curious?
Here we go.
The study included patients with coronary artery stenosis ≥70% and OSA (apnoea-hypopnoea index ≥ 15).
It showed that the treatment of OSA was associated with a decrease in the occurrence of cardiovascular events in CAD.
Examples of cardiovascular events included:
- cardiovascular death,
- heart attack,
- hospitalization for heart failure,
- or need for coronary revascularization (see also How are OSA and coronary heart disease related?).
A group of patients was treated with CPAP (21 patients) or upper airway surgery (4 patients).
And another group (29 patients) refused treatment.
Interestingly, the two groups were similar regarding other characteristics that may have influenced coronary heart disease such as:
- age,
- body mass index,
- smoking history,
- hypertension,
- hypercholesterolemia,
- diabetes mellitus,
- number of diseased vessels,
- left ventricular ejection fraction,
- and coronary heart disease therapy.
What was finally observed?
The treatment of OSA led to:
- a decrease in the occurrence of new cardiovascular events,
- an increase in the time to such events.
So, the results were encouraging.
Let’s now talk about another cardiovascular disease: irregular heartbeat (cardiac arrhythmias).
You may be interested to discover how CPAP affects your arrhythmias when you are treated for OSA.
Just scroll down.
Does treatment of OSA reduce cardiac arrhythmias?
Only studies can answer such questions.
And a study indeed there is.
What does it show?
That if you suffer from OSA, then your risk of arrhythmias decreases with CPAP therapy.
Even if you suffered from frequent occurrences of irregular heartbeat, this would decrease quite fast.
Another study also showed that:
- if you suffer from atrial fibrillation and OSA,
- and if you get treated for your arrhythmia,
- the return of your cardiac atrial fibrillation will decrease from 80% to 40% if you are on CPAP35.
Worthy of interest is also the fact that among patients with a pacemaker, the prevalence of undiagnosed sleep apnea is 59%.
Since we spoke about pacemakers, do we know whether treatment by CPAP affects their use?
Next …
Does night treatment of OSA reduce need of a pacemaker?
You have seen that arrhythmias decrease after CPAP treatment of sleep apnea.
What about the use of a pacemaker to control arrhythmias?
Can its use be decreased if OSA gets treated?
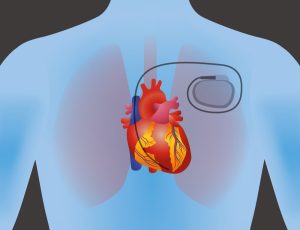
Unfortunately, there are currently no data to answer this question.
As we wait for science to progress, let’s look at other effects of OSA.
Erectile dysfunction (ED), for instance, affects your quality of life.
It is also linked to OSA.
With that in mind, let’s roll right in.
Can treating OSA improve your erectile dysfunction (ED)?
If you have stayed with us all the way from the beginning of this guide, then you are almost an expert on OSA therapies ?.
So, you know that the established first-line therapy for OSA is CPAP.
It is thus no surprise that most of the studies on OSA patients suffering from ED have been done using CPAP.
And what about the results?
Unfortunately, they are inconsistent:
- Some studies show improvement in ED and hormonal levels (e.g. testosterone).
- Others instead show improvement in ED only.
- Finally some show neither improvement in testosterone levels nor in sexual function.
Some preliminary encouraging results come from uvulopalatopharyngoplasty (UPPP).
This surgical procedure has shown encouraging results.
The outcomes are actually better than both CPAP and mandible advancement procedures. But more studies are required.
Another way CPAP can improve your quality of life, is by treating your OSA when you suffer from depressive symptoms.
Read on to find out.
Does treating OSA decrease depressive symptoms?
A 2007 study showed encouraging results.
Patients suffering from OSA and treated with CPAP showed a marked improvement in their symptoms of depression.
This was both true at short-term and long-term follow-up periods, indicating that results were lasting.
Diabetes Type 2 is the last OSA associated disease we want to touch upon.
Stay with us if you want to learn how CPAP affects its symptoms.
Can OSA treatment help diabetes type 2 patients or patients with abnormal glucose levels?
If you suffer from these 2 diseases, you will be relieved to know the news are somewhat good.
Several studies show that CPAP can improve your cells’ ability to use glucose especially if:
- You are compliant with the treatment meaning that you correctly follow medical advice,
- and if you use CPAP >4 hours per night.
But, these studies focused on individuals with:
- normal blood glucose concentrations
- or patients with pre-diabetes.
Unfortunately, strong evidence is lacking for the impact of CPAP on glucose levels, in patients with Type 2 diabetes.
Now that we have completed this detour through OSA’s related health effects.
Let’s now go back to CPAP.
We had mentioned that it has some side effects.
Curious?
Then jump right in!
What are the side effects with CPAP and what are the solutions?
Despite its effective use in treating sleep apnea, CPAP can create some frustrations
Although serious side effects are extremely rare, there are minor problems which are quite frequent:
- machine noise,
- pressure from masks or straps,
- air leaks from mask,
- air leaks from your mouth,
- cold face or nose,
- claustrophobia,
- dry mouth or throat,
- air pressure is too high,
- skin irritation on your face,
- mask coming off your face,
- chest discomfort,
- difficulty breathing,
- nosebleeds,
- a dry nose,
- a stuffy nose,
- a runny nose,
- a headache,
- bloating.
It will thus not come as a surprise that the main problem with CPAP is…
…low acceptance and adherence to treatment.
In other words, although it is very effective, the risks are high of you not complying with what your sleep specialist advises.
And you will be likely to use it irregularly and/or stop using it after a few years. …. and guess what?
….This will decrease its effectiveness.
The next sections will look in more detail at:
- Some common problems that may influence your acceptance
- and also check some possible solutions.
But before we do that, remember that it may take some time to:
- find the right settings
- and to get used to wearing a mask at night.
Your sleep doctor will help you identify and correct any issues and adjust settings.
Let’s look at the first culpright of low compliance.
Air leaks
One frequent issue is air leaks.
You need to address this problem if:
- you complain about them,
- the machine cannot maintain enough pressure,
- they exceed the machine’s threshold,
- your eyes are dry or teary due to some of the air leakages.
Some solutions include:
- cleaning the mask since the softer and cleaner the silicone, the better its skin adhesion;
- changing type of mask if the above solutions are not satisfactory, if the mask is worn out or if it’s the wrong size;
- checking and adjusting mask’s positioning, as well as its straps, with air pressure on.

If you are without teeth then wearing your dentures at night is important.
If you feel significant discomfort from a dry mouth, then a likely cause is mouth leaks.
You can try to use a chin strap.
You should consider that everyone has different face shapes. Hence, changing mask may be a good solution.
When changing mask, you should seek help from your doctor and supplier to find the best mask for you.
Let’s now check another source of discomfort.
Skin irritation, sores or blisters
CPAP masks exert prolonged pressure on the skin.
So here is the (expected) kicker..
… skin pain and adverse effects
Since pressure is the cause, then:
- ensure that the mask is properly fitted over your face by adjusting pads and straps;
- most masks are adjustable, so take advantage of this;
- clean the mask daily. A cleaner silicone ensures a better seal and you will not need tightening the straps too hard;
- consider also changing your mask especially if your weight has changed considerably;
- think about using a nose patch;
- if you have sores, blisters or your skin has deteriorated significantly, tell your doctor and stop CPAP until skin healing.
Dry Mouth
Breathing through your mouth a whole night is not pleasant because it gets dry.
But it gets worse with some CPAP devices.
Consider:
- switching to a mask covering your mouth and nose,
- use a CPAP-heated humidifier.
How does the latter work?
Simple… it connects to the air pressure machine to increase the level of moisture in the air.
Dry, stuffy, runny nose
A dry nose can be due to a leaky mask.
Ensure that it fits well. A good test is to see whether you need (or not) to tighten your straps.
If you have to tighten straps too often, then consider changing your mask. It may not fit properly.
Use a humidifier. This is connected to the CPAP machine. Increase the level of moisture if the problem persists.
Change from a nasal pillow to another type of mask to reduce the flow of direct air.
A nasal saline spray before falling asleep may also help.
Pressure is perceived as too high, difficulty in exhaling
You will require some time to adapt to CPAP.
So that will need …. yes, you know …. a good deal of patience.
Though, you can also address the pressure issue via the ramp feature. This is present on individual devices.
It allows you to fall asleep with a lower pressure level. This is then gradually increased during the night, up to a final level set by your doctor.
If you wake up at night, you can also turn the machine off and on, so that the process starts all over again.
If this does not help, there are other solutions that you can discuss with your doctor.
An example is a bi-level positive airway pressure (BPAP) machine.
A bi … what?
It is a sophisticated word for a device that:
- continuously adjusts the pressure it delivers,
- so that air pressure is higher when you breathe in than when you breathe out.
Feeling claustrophobic
You can deal with this issue if you approach it gradually.
You will see that it usually decreases over 3 months.
Try to use the mask regularly, even for a short time, so that your tolerance threshold increases.
At first, you can use it while you are awake without the straps.
Then you should try wearing it with the straps on.
Finally, you will have to add the hose to the mask, at first without the straps.
You should then try to use the CPAP machine and once you will feel more comfortable also use the straps.
Finally, the last step….. you have probably guessed already.

…….. you need to sleep with the mask on, straps attached and CPAP machine turned on.
If this approach does not yield good results, then talk to your doctor or CPAP supplier.
There exist other types of masks, coming in different sizes and shapes such as nasal pillows.
These could be a solution because they make you feel less claustrophobic than a full face mask.
Why?
Because they do not cover your mouth. Albeit they also have straps that stretch across your forehead and cheeks.
Difficulty getting used to the CPAP device
Just as with claustrophobia, try to get used to the CPAP mask by wearing it when awake.
Do not force yourself to wear it for a long time right from the start.
Increase the amount of time gradually.
Then begin using the device turned on, connected to its tubes when awake and then when napping.
Finally, begin using it during your night’s sleep.
You may temporarily take some sleeping pills to ensure falling asleep more quickly. Else consider going to bed somewhat later (for the same reason).
After some time, you will feel whether mask and pressure are right for you or not.
Too noisy
Since most new generation devices are almost silent, this should not be a frequent occurrence.
So, when it happens, what may it be due to?
Here are some causes:
- improperly closed humidifier,
- clogged device air filter (it should be clean and unblocked)
- punctured tubing,
- defective engine,
- leaks around the mask,
Try to find a solution by liaising with your sleep specialist or CPAP supplier to:
- understand how to clean your mask and hose,
- ensure that the whole device is working as it should.
Also, consider placing the machine:
- as far as possible from the bed (you may need extra tubing for that),
- on a surface that can reduce noise levels: a mousepad, a strip of cloth …
Other solutions entail:
- Wearing earplugs,
- using a white noise machine to mask the noise. So, the device would make a random pleasant sound (called white noise). Examples include wind blowing through trees or a rushing waterfall.
If all else fails, then consider changing the machine.
What are the effects of CPAP therapy on your jaws and teeth?
Once you have fine-tuned your CPAP therapy to decrease the sources of discomfort, then you are all set, and there is nothing else to worry about, right?
Wrong!
A study over 2 years showed that CPAP therapy can affect the position of your jaws and teeth.
For instance, some patients had less prominent lower or upper jaws (“reduced maxillary and mandibular prominence”).

Another study showed a decrease in the premolar region’s occlusal points. These are the contacts points between opposing teeth’s surfaces.
In this study, patients had also been using CPAP over 2 years.
Hence it is important that you see your sleep specialist regularly. This will ensure optimal results with your CPAP therapy.
CPAP and dental appliances: results and comparisons
How do sleep apnea results obtained with CPAP compare to those obtained with mouthpieces?
Head to head studies comparing the two therapies during overnight sleep studies provide the answers to this question.
And so, the answer is that…
……… although CPAP shows greater efficacy, and can reduce AHI by 6 events/hour, final results are comparable.
Also, a study with 103 patients using (randomized to) either CPAP or dental appliances, showed that quality of life improved significantly and similarly irrespective of the treatment.
Feeling a little puzzled by these findings?
The explanation is that patients use dental appliances more easily. So, they end up wearing them for more extended hours during their night’s sleep.
Even if you show better response when using CPAP, this will be offset by your tendency:
- to stop using it
- or using it less regularly.
Patients are twice less likely to discontinue using oral appliances than CPAP.
Now, assuming that your compliance is excellent, do the above therapies put an end to your concerns?
Next…
Do dental appliances or CPAP cure sleep apnea?
A short answer is … no, unfortunately
That is because neither dental appliances nor CPAP:
- Can address the main causes
- or bring about the structural changes
that may resolve your sleep apnea.
These include:
- correcting your deviated septum by undertaking surgery
- treating your allergies
- weight loss because you go on a diet
- ….

So, they are not cures since your sleep apnea will return as soon as you stop using them.
The predisposing factors are still there.
But, as long as you use them, both dental appliances and CPAP can help you:
- maintain your airways open
- and improve or fully resolve your sleep apnea.
In a way, CPAP and dental appliances are like a pair of glasses. They can improve your quality of life without changing the underlying problem.
What happens when you stop using CPAP or dental appliances?
Symptoms like fatigue, daytime sleepiness will return more or less rapidly
Why not immediately?
Because the use of CPAP or dental appliances may have decreased the swelling in your airways.
As snoring and sleep apnea gradually return, so does the swelling, leading to a vicious circle.
The circle is vicious ☹ because:
- as the swelling worsens,
- so do the snoring and sleep apnea,
- which in turn increase the swelling.
And that’s all folks!
Final remarks
To reach omniscience about OSA, you have one more chapter to read.
This is “Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.”
It will walk you through a more invasive approach to treating sleep apnea.
Now, if you have not seen the previous articles, then check the links here below. They are also important on your path towards OSA wisdom ?.
Chapter 3: Diagnosis of Obstructive Sleep Apnea (OSA).
Obstructive Sleep Apnea: The Definitive Guide for 2020.
Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects.
Chapter 2: Doctors Who Diagnose and Treat Obstructive Sleep Apnea.
SUTTON PLACE DENTAL ASSOCIATES ON THE WEB





SLEEP APNEA
[menu_in_post_menu menu=11 menu_class=”menuinpost” style=”list”]
